Stomach
Chronic peptic ulcer
Chronic peptic ulcer represents a deep loss of substance, being associated most often with Helicobacter pylori-induced hyperclorhidric chronic gastritis and chronic NSAID use.
Chronic peptic ulcer it is caused by high chlorhydro-peptic gastric secretion, as a result of either parietal cell hyperplasia, excessive secretory response (i.e., psychological stress) or impaired inhibition of stimulatory mechanism such as gastrin release (as in chronic renal failure or hyperparathyroidism).
In more than 95 % of cases, chronic peptic ulcer is located on the lesser curvature of the stomach and in the proximal duodenum.
Less often, it can affect the esophagus (in Barrett esophagus), Meckel diverticulum (with ectopic gastric mucosa), gastrojejunal anastomosis or the small bowel (in Zollinger-Ellison syndrome).
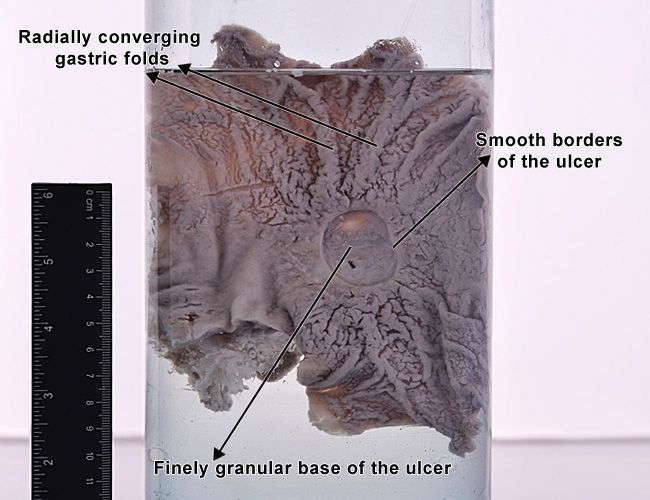
Gastric chronic peptic ulcer
Macroscopically, the loss of substance is round or oval, has 2 - 4 cm in diameter and slightly elevated borders. The base is clean, finely granular. The gastric wall surrounding the ulcer is endured, because of the fibrosis which involves the base of the ulcer and spreads beneath the surrounding mucosa. Being retractile, the fibrosis manages to "pull" the gastric mucosa towards the base of the ulcer, so that gastric mucosal folds converge radially around the loss of substance (this feature is not seen in ulcerated malignant gastric tumors).
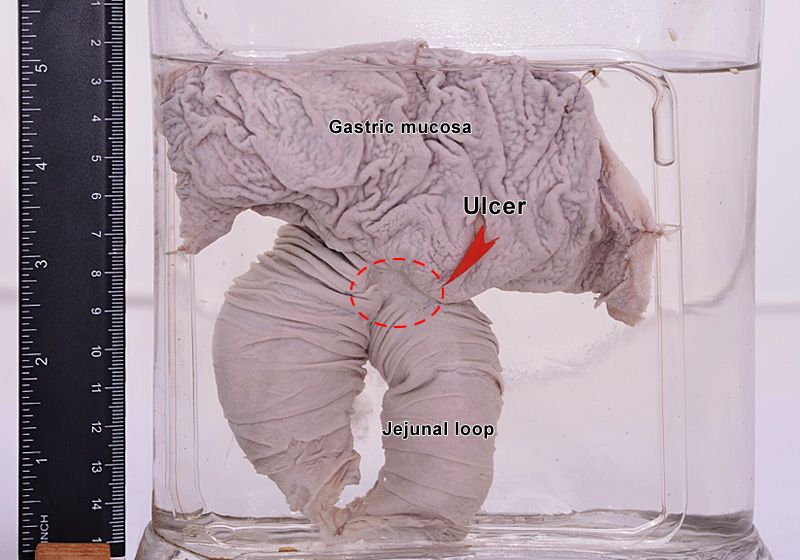
Stomal chronic peptic ulcer
Chronic peptic ulcer involving the gastrojejunal anastomosis. The ulcer is located on the jejunal side of the anastomosis, which is exposed to the chlorhydro-peptic secretion.
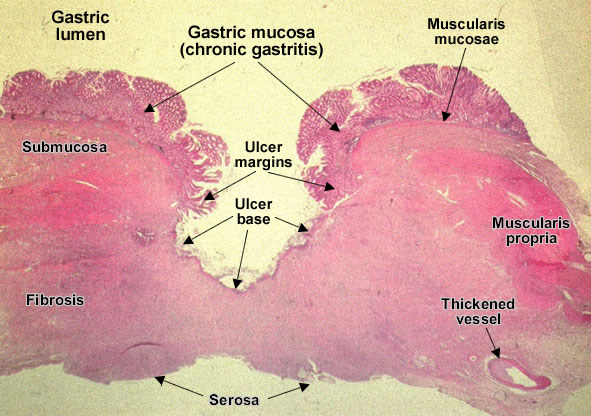
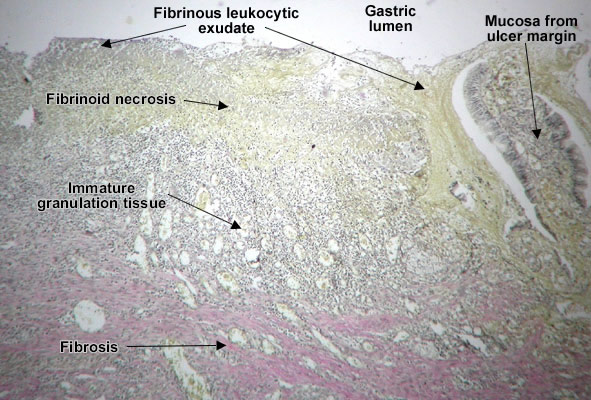
Chronic peptic ulcer (stomach) is a mucosal defect which penetrates the muscularis mucosae and muscularis propria, produced by acid-pepsin aggression. Ulcer margins are regular, slightly elevated due to adjacent chronic gastritis. During the active phase, the base of the ulcer shows 4 zones : inflammatory exudate, fibrinoid necrosis, granulation tissue and fibrous tissue. The fibrous base of the ulcer may contain vessels with thickened wall or with thrombosis. (H&E, ob. x7)
Chronic peptic ulcer (stomach).
During the active phase, the base of the ulcer shows 4 zones :
- inflammatory exudate - at the lumen (cell debris and neutrophils)
- fibrinoid necrosis (yellow in van Gieson staining and pink in H&E)
- granulation tissue (see Granulation tissue)
- mature fibrous tissue (abundant collagen - red in van Gieson staining and pink in H&E, profound, spreading beneath ulcers margins, producing mucosal retraction - radiating folds). This fibrous layer may contain vessels with thickened walls or with thrombosis. (H&E, ob. x10)
Complications of Chronic peptic ulcer
Upper gastrointestinal bleeding - represents the most frequent complication of a chronic peptic ulcer, which occurs in the active phase of the ulcer, caused by the erosion of an arterial wall.
Perforation - represents a surgical emergency in which the loss of substance extends beyond the gastric serosa, resulting in the communication between the stomach and the peritoneal space.
Penetration - in the evolution of ulcers, inflammation of serosa leads to adhesions with adjacent organs (liver, pancreas, greater omentum) so that, when the loss of substance exceeds serosa, the ulcer base is represented by the parenchyma of that organ, with no communication with the peritoneal cavity.
Gastric stenosis - appears in chronic ulcers with extensive, abundant fibrosis.
Malignant transformation - represents a very rare complication (less than 1 % of the cases). In the malignant area, the ulcer's borders are irregular, anfractuous. This complication is controversial, as some believe that the ulcer represents in fact an ulcerated form of gastric carcinoma.